Fatty Liver, NAFLD and NASH
What is Fatty Liver, NAFLD and NASH?
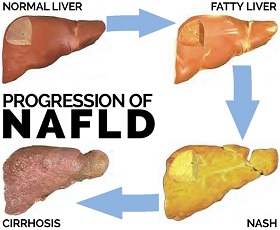
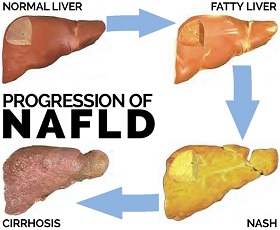 Nonalcoholic Fatty Liver Disease (NAFLD) is the buildup of extra fat in the liver that is not caused by alcohol. It is named for a grouping of liver abnormalities/diseases ranging from the relatively harmless fatty liver to Nonalcoholic Steatohepatitis (NASH) to cirrhosis.
Nonalcoholic Fatty Liver Disease (NAFLD) is the buildup of extra fat in the liver that is not caused by alcohol. It is named for a grouping of liver abnormalities/diseases ranging from the relatively harmless fatty liver to Nonalcoholic Steatohepatitis (NASH) to cirrhosis.
It is normal for your liver to contain some fat. However, if more than 5% to 10% of your liver’s total weight is fat, then it is called a fatty liver (steatosis) – the first stage of Nonalcoholic Fatty Liver Disease (NAFLD).
According to the American Liver Foundation, up to 20% of Americans have fatty liver. The good news is that fatty liver is a totally reversible condition. Fatty liver is relatively harmless. It typically can be reversed with weight loss, healthy changes in diet, exercise, and by only taking medicines that are needed and their dosing recommendations followed – so fewer toxins enter the body and less stress is put on the liver.
When a fatty liver is accompanied by varying degrees of inflammation and scarring (fibrosis), you then have Nonalcoholic Steatohepatitis (NASH), a more severe form of NAFLD. Unlike fatty liver, NASH is not considered relatively harmless. Instead, NASH is considered a liver disease with the potential to progress to cirrhosis, which can then lead to liver failure. When inflammation occurs, the liver doesn’t work efficiently and liver cells can be destroyed. This can lead to scarring of the liver. When the scarring is more advanced and irreversible, it is called cirrhosis. Only a small portion of people with fatty liver will develop NASH.
NAFLD is the leading cause of chronic liver disease.
NAFLD is the third most common reason for liver transplants in the United States.
Cirrhosis, the third stage of NAFLD is the 12th leading cause of death in the United States.
What Causes Fatty Liver, NAFLD and NASH?
The liver is involved in the metabolism of fat. This process can be disrupted by a variety of factors, including certain types of diseases, poor diet, certain medications and some toxins. When this process of fat metabolism is disrupted, the fat can accumulate in the liver in excessive amounts, thus resulting in a fatty liver, the first stage of NAFLD.
Who Is At Risk for Fatty Liver, NAFLD and NASH?
 Fatty liver is most commonly found in people who consume excessive amounts of alcohol, who are obese, as well as those who are diabetics (Type 2).
Fatty liver is most commonly found in people who consume excessive amounts of alcohol, who are obese, as well as those who are diabetics (Type 2).
For those who are obese, fatty liver is most frequently found in those that carry excess fat mainly around their midsection.
For those with diabetes, fatty liver is most frequently found in those who have Type 2 diabetes.
Common risk factors for the development of fatty liver and NASH:
- Obesity
- Diabetes (Type 2)
- Hyperlipidemia [high levels of lipids (fats) in the blood]
- High cholesterol
- Rapid weight loss
- Starvation
- Use of steroids, estrogen, amiodarone (a heart medication), tamoxifen (medication used for breast cancer), methotrexate (a type of chemotherapy)
- Weight reduction surgery – gastroplasy or gastric bypass
What are the Signs and Symptoms for Fatty Liver, NAFLD and NASH?
Most people with fatty liver or NASH have no symptoms. When symptoms do occur, they are not dramatic and typically not specific. Fatigue and weakness are examples of these such symptoms. Sometimes a patient will complain of pain or discomfort over the area of the liver, which could be caused by the stretching of the liver covering due to the increase in fat deposits and inflammation. The pain is usually dull and aching, not intense, sudden or severe. There is also no predictable pattern when the pain occurs.
How is Fatty Liver, NAFLD and NASH Diagnosed?
During an exam a doctor may detect an enlarged liver and signs of cirrhosis like ascites (fluid buildup in the abdominal cavity). An enlarged spleen might also be present but only in people with NASH. There is no single test that can accurately diagnose fatty liver or NASH. A diagnosis of NASH is made only after all other causes of fatty liver and causes of elevated liver enzymes have been excluded.
Blood work can be done to test for any abnormalities. Typically elevations in liver enzymes - whereby the level of ALT elevation is higher than the level of AST - elevation could be an indicator of fatty liver or NASH.
 Ultrasounds can also be performed to diagnose fatty liver. However, an ultrasound needs a skilled operator. In addition, the sensitivity of the scan is decreased in people with high amounts of abdominal fat. A CT (computerized tomography) scan could be performed as well and may even measure the degree of fat in the liver, but this determination can be hampered if there are any liver iron deposits. Imaging studies can detect the presence of fat in the liver but not the severity.
Ultrasounds can also be performed to diagnose fatty liver. However, an ultrasound needs a skilled operator. In addition, the sensitivity of the scan is decreased in people with high amounts of abdominal fat. A CT (computerized tomography) scan could be performed as well and may even measure the degree of fat in the liver, but this determination can be hampered if there are any liver iron deposits. Imaging studies can detect the presence of fat in the liver but not the severity.
Therefore, one can presume a diagnosis of fatty liver or NASH based on signs of insulin resistance, elevated ALT levels for a long duration, signs of fatty liver through imaging and exclusion of other causes of elevated ALT levels and fatty liver.
Only a liver biopsy can definitively diagnose a fatty liver and NASH as well as the amount of fatty deposits, degree of inflammation and extent of damage to the liver.
What is the Treatment for Fatty Liver, NAFLD and NASH?
The treatment of fatty liver and NASH depends on the cause. Patients who are overweight or obese can usually normalize their elevated liver enzymes, decrease some of the liver enlargement and the amount of fat in the liver through weight reduction. If weight reduction is done early on after diagnosis, scarring and cirrhosis of the liver can possibly be prevented altogether. Keep in mind that weight loss must be achieved slowly through a doctor's recommended plan of diet and exercise. Weight loss should not be accomplished through quick or fad dieting, as this can actually exacerbate disease progression. Also, weight loss must be maintained or the disease may come back.
If cirrhosis is not already present and it was determined that the fatty liver or NASH was caused by medication or a toxin, if one discontinues exposure to these causes the condition, generally, can be reversed.
For Type 2 diabetics who have developed fatty liver or NASH, controlling sugar levels is important but will generally not improve liver abnormalities – for those that are overweight, weight reduction is the only effective option.
For those people who are not overweight, there is no specific treatment for fatty liver or NASH. There are medications that are being evaluated for this group. Speak with your doctor about this. Some alterations in diet, such as correcting protein deficiencies and avoiding carbohydrate and excess fat, could be effective.
For those with NASH who have developed cirrhosis, they should be evaluated for possible liver transplant.
This information is intended for educational purposes only and should not be used in any other manner. This information is not intended to substitute for informed medical advice. You should not use this information to diagnose or treat a health problem or disease without consulting with a qualified health care provider.
Suggested Articles:
 Nonalcoholic Fatty Liver Disease (NAFLD) is the buildup of extra fat in the liver that is not caused by alcohol. It is named for a grouping of liver abnormalities/diseases ranging from the relatively harmless fatty liver to Nonalcoholic Steatohepatitis (NASH) to cirrhosis.
Nonalcoholic Fatty Liver Disease (NAFLD) is the buildup of extra fat in the liver that is not caused by alcohol. It is named for a grouping of liver abnormalities/diseases ranging from the relatively harmless fatty liver to Nonalcoholic Steatohepatitis (NASH) to cirrhosis. Fatty liver is most commonly found in people who consume excessive amounts of alcohol, who are obese, as well as those who are diabetics (Type 2).
Fatty liver is most commonly found in people who consume excessive amounts of alcohol, who are obese, as well as those who are diabetics (Type 2).  Ultrasounds can also be performed to diagnose fatty liver. However, an ultrasound needs a skilled operator. In addition, the sensitivity of the scan is decreased in people with high amounts of abdominal fat. A CT (computerized tomography) scan could be performed as well and may even measure the degree of fat in the liver, but this determination can be hampered if there are any liver iron deposits. Imaging studies can detect the presence of fat in the liver but not the severity.
Ultrasounds can also be performed to diagnose fatty liver. However, an ultrasound needs a skilled operator. In addition, the sensitivity of the scan is decreased in people with high amounts of abdominal fat. A CT (computerized tomography) scan could be performed as well and may even measure the degree of fat in the liver, but this determination can be hampered if there are any liver iron deposits. Imaging studies can detect the presence of fat in the liver but not the severity.