Ascites
- What is Ascites?
- Causes
- How Do I Know if I Have It?
- How Do I Know What is Causing My Swelling?
- Treatment
- Suggested Articles
What is Ascites?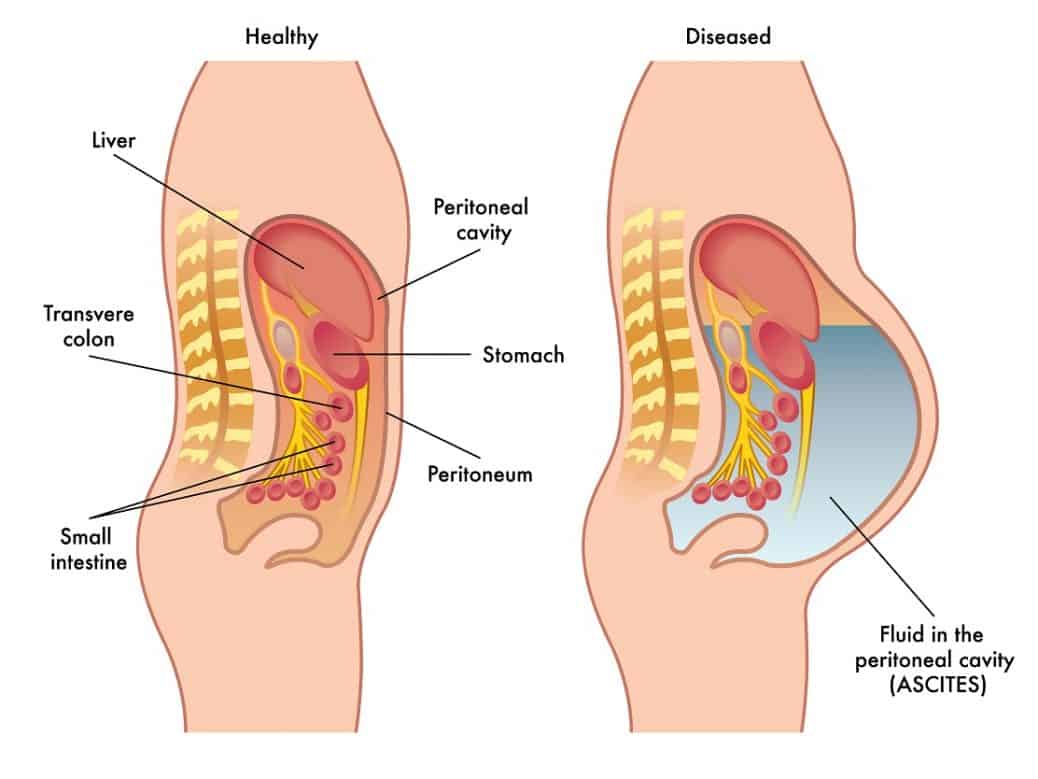
Ascites is the presence of excess fluid in the peritoneal cavity, which is the space between the abdominal organs and the skin. As a result of this fluid buildup, the abdomen swells and distends.
Causes
While liver disease – specifically cirrhosis – is the most common cause, it can also have other causes, such as cancers, congestive heart failure or kidney failure. Here, however, we’ll be concentrating on ascites as a result of liver disease.
With liver disease, buildup of scar tissue can prevent blood from flowing freely through the liver, resulting in blood being backed up in the portal vein. It may happen as a result of swelling of this portal vein causing portal hypertension. Swelling of the portal vein can then block the lymph channels causing the lymph to spill into the abdomen.
Ascites may also happen as a result of low blood albumin levels. Blood albumin performs many functions, including maintaining the ‘osmotic pressure’ that causes fluid to remain within the blood stream instead of leaking out into the tissues. Liver disease is a major cause of low albumin since a diseased liver does not product sufficient albumin. Thus, low albumin levels can cause plasma to diffuse from the veins and arteries into the tissues, thus leaking into the abdomen.
Ascites is usually a sign of severe liver disease and must be clearly distinguished from other reasons for abdominal distention.
How Do I Know If I Have It?
Ascites may be asymptomatic (having no symptoms) or a person may complain of increased abdominal width, becoming full quickly upon eating or breathing difficulty, depending upon the amount of fluid that has accumulated.
A physician may perform various physical tests. Upon physical examination a doctor may determine that a person has ascites if there is presence of the following:
- If abdominal distention, or bloating of the belly, is present.
- The sides of the abdomen, or flanks, are pushed outward.
- When percussion is done over the abdomen and percussion note is tympanitic over the umbilicus (belly button) and dull over the lateral abdomen and flank areas (sides of the abdomen). This detection of tympany can be caused because the bowel floats to the top of the fluid in the abdomen.
- If there is a shifting in dullness. When percussion is performed while the patient is laying on his/her back and then percussion is performed with the patient lying on his/her side, and the area of dullness shifts such that the area of tympany shifts to the top.
- If a wave like motion is detected when the doctor places one hand on the flank and taps the opposite flank, fluid may be detected.
If a physical examination does not definitively show that the swelling is caused by excess fluid, a sonogram, ultrasound or CT (computerized tomography) scan may be performed.
How Do I Know What Is Causing My Swelling?
Blood work may be helpful in determining the cause of the swelling, as a complete metabolic panel may detect any injury to the liver as well as level of liver function.
In some cases, to determine the cause of the excessive abdominal fluid, it must be removed and analyzed through paracentesis. Paracentesis involves placing a needle into the abdomen where the fluid is accumulated to draw out fluid for examination. If the ascites is due to liver disease, the fluid will be clear, yellow, uninfected and have a low cell count.
If a fever accompanies the abdominal swelling, a bacterial infection can also be involved and must be treated immediately. Abdominal paracentesis with analysis of the ascitic fluid should be done in patients with new onset ascites, those requiring hospitalization because of ascites and those whose condition deteriorates during hospitalization.
Treatment
The treatment depends on its cause. If portal hypertension is the cause, medical management using diuretics and salt restriction is often effective in portal hypertensive patients.
Most patients who have ascites as a result of cirrhosis respond to dietary sodium restriction and diuretics. Diuretics can increase the amount of urine excreted, thus decreasing the amount of retained fluid. Diuretics and their usage must be prescribed by a physician.
If diuretics and salt restriction are not effective, in some cases, doctors may perform paracentesis to draw off the fluid from the abdomen. A few liters of fluid can be removed at a time.
In other cases where the paracentesis procedure is repeatedly required to prevent the re-accumulation of fluid, the physician may resort to other means. A transjugular intrahepatic portosystemic shunt (TIPS) may be implanted to redirect the fluid and provide relief. This procedure is performed by a vascular radiologist.
This information is for educational purposes only and should not be used in any other manner. This information is not intended to substitute for informed medical advice. You should not use this information to diagnose or treat a health problem or disease without consulting with a qualified health care provider.
Suggested Articles
- The High Infection Risk Associated with Cirrhosis
- Important Facts About Salt and Cirrhosis
- The Catch-22 of Chronic Liver Disease
- The High Infection Risk Associated with Cirrhosis
Bruce, Cara and Montanarelli, Lisa. The First Year: Hepatitis C An Essential Guide for the Newly Diagnosed. New York: Marlowe & Company, 2007.
Cohen, O.M.D., L.Ac., Misha Ruth and Gish, M.D., Robert. The Hepatitis C Help Book. New York: St. Martin’s Griffin, 2007.
Everson, M.D., Gregory and Weinberg, Hedy. Living with Hepatitis C: A Survivor’s Guide. New York: Hatherleigh Press, 2009.
Fontana M.D., Robert. "TIPS Procedure: Effects on Kidneys, History and More" http://www.hepatitis-central.com/hcv/whatis/shunt.html. Retrieved October 7, 2010.
Nabili, M.D. Siamak. "Ascites" http://www.medicinenet.com/ascites/article.htm. Retrieved on October 7, 2010.
Palmer, M.D., Melissa. Dr. Melissa Palmer’s Guide to Hepatitis & Liver Disease. New York: Avery Trade, 2004.
Washington, Harriet A. Living Healthy with Hepatitis C. New York: Dell Publishing, 2000